T, a student at a Colorado medical school, can count on one hand the things she’s learned about cannabis and psychedelics from her professors.
“We’ve had probably two hour-and-a-half lectures on drugs of abuse, which included weed and psychedelics,” she said, “and a decent amount of information about the use of ketamine on PTSD in our psych course.”
Beyond that, T said, cannabis has been “brought up a couple times,” including its potential to fight nausea and stimulate appetite. She may learn more in her third and fourth years, but “I’m a little bit disappointed in how much we’ve learned so far.”
Recreational cannabis has been legal for a decade in Colorado; medical uses have been legalized for nearly a quarter-century. Weed and psychedelics such as shrooms — decriminalized in Denver five years ago and statewide in 2022 — are widely used.
Despite their ubiquity, doctors are ill equipped to counsel patients on the potential harms, benefits or side effects of these legal drugs. There are no standard curricula for medical students in Colorado or the U.S. and no requirements that physicians be educated about them.
“It’s a bit taboo to be talking about drugs,” T said of the medical school setting. She did not feel comfortable providing her name or the name of her institution, which has strict policies on media and a prohibition on cannabis. Students are routinely drug tested.
“They definitely have left me with a lot of questions,” T said, “and I know my peers feel the same way.”
‘Do their own homework’
A 2017 study found that just 9% of medical schools had anything about medical marijuana in their curricula. Titled “Physicians-in-training are not prepared to prescribe medical marijuana,” the report “highlights a fundamental and potentially growing mismatch between the legalization of medical marijuana at a state level and the ability of physicians to properly address patients’ questions about medical marijuana or to appropriately prescribe it,” authors wrote.
There does not appear to be more recent data about medical school curricula than the now-seven-year-old study, published before many states legalized cannabis and/or psychedelics.
“The AAMC does not have any data on cannabis or psychedelics in medical school curriculum,” wrote a spokesperson for the Association of American Medical Colleges, in response to an interview request. “Neither the AAMC nor the LCME (Liaison Committee on Medical Education), the accrediting body for medical education programs, prescribe a specific curriculum. Each medical school designs its own.”
A spokesperson for the Federation of State Medical Boards likewise wrote, “We do not have any information on this, as our member state medical boards do not have any jurisdiction over med school curricula.”
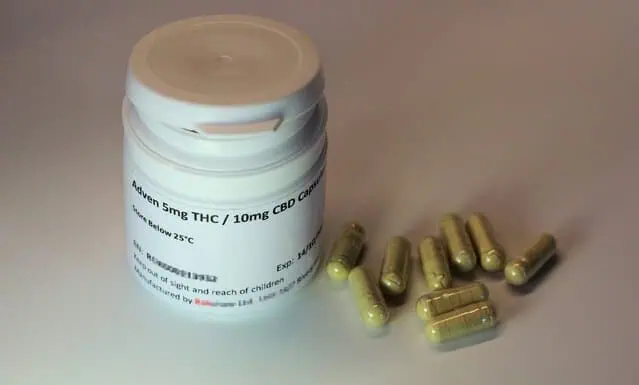
The board overseeing medical licenses for doctors in Colorado devotes three of its 107-page policy guidelines to recommendations for prescribing “marijuana as a therapeutic option.” Physicians should consider patient and family history, drug interactions and other physical and psychological conditions, the guidance states, and “may subsequently counsel the patient regarding the pros, cons, risks, benefits, alternatives, and other relevant considerations around a recommendation for marijuana as a therapeutic agent.”
The rules for cannabis are “the same for any pharmaceutical drug that comes to market,” said Katie O’Donnell, director of communications for the Colorado Department of Regulatory Agencies, which oversees the medical licensing board. “A medical provider would need to do their own homework.”
Behind the research
State statute does mandate that doctor’s give advice based on research, O’Donnell said, “but they don’t really go into detail on what you can or can’t say to a patient.”
That’s partly because so little is known about cannabis and psychedelics. Federal prohibition has made doing research difficult, which may prevent physicians from sharing what is suspected but not confirmed about illicit drugs.
T has been taught what to say if patients have questions about recreational drugs, including cannabis.
“The acceptable response is, ‘I don’t know a lot about this. Let me do my research and get back to you,’” she said, which is also how doctors are trained to respond to questions about pharmaceuticals they are unfamiliar with.
T is looking forward to the anticipated reclassification of cannabis at the federal level and the launch of therapeutic psychedelic programs in Colorado, which may spur more research into the positive potential of the drugs as well as the unknown side effects and drug interactions — information that will ultimately make her a better doctor.
“We’ll have a lot more answers for people,” she said. “And not be so afraid to talk about it.”
Read more about recreational drugs from Boulder Weekly
